2. 开滦总医院 核磁室, 河北 唐山 063000;
3. 唐山市协和医院 超声室, 河北 唐山 063000;
4. 唐山市协和医院 放射科, 河北 唐山 063000
2. Nuclear Magnetic Laboratory of Kailuan General Hospital, Tangshan 063000, Hebei, P. R. China;
3. Department of Ultrasound, Tangshan Xiehe Hospital, Tangshan 063000, Hebei, P. R. China;
4. Radiology Department, Tangshan Xiehe Hospital, Tangshan 063000, Hebei, P. R. China
甲状腺结节是临床上常见的甲状腺疾病,其在我国的发病率约为10%,多数患者为良性结节,但也有部分患者为恶性结节,若未能及时诊治,易因其早期生长较快或淋巴转移等而增加治疗难度,导致预后不良[1]。目前,计算机断层扫描(computed tomography, CT)、磁共振成像(magnetic resonance imaging, MRI)是临床上重要的影像学手段,二者逐渐被应用于甲状腺疾病检查中,且随着医疗技术的发展与成熟,其检查价值逐渐提高并受到人们的关注和重视,但关于CT、MRI联合鉴别良恶性甲状腺结节的报道较少[2, 3]。对此,本研究通过给予甲状腺结节患者CT、MRI检查,以病理结果为对照,探讨CT、MRI对良恶性甲状腺结节的鉴别价值。
1 资料与方法 1.1 一般资料选取2015年3月至2018年3月本院收治的甲状腺结节患者150例,依据病理结果分为恶性48例、良性102例,本研究经伦理委员会审批通过。纳入标准:(1)病理结果证实为良恶性甲状腺结节且为单发性结节;(2)年龄>18岁、无精神病病史;(3)就诊前1个月无内分泌、手术、化疗、放疗等影响本研究结果的治疗史;(4)签署知情同意书。排除标准:(1)妊娠期、哺乳期女性;(2)有CT、MRI检查禁忌症;(3)有心、肝、肾等严重性疾病;(4)不配合检查或资料收集不完整。恶性:年龄34~68岁、体质量指数17.58~28.46 kg/m2、结节直径12~76 mm,乳头状癌38例、滤泡状癌10例、髓样癌2例,淋巴结转移60例。良性:年龄32~67岁、体质量指数17.52~28.51 kg/m2、结节直径10~74 mm。良恶性甲状腺结节患者性别、年龄、体质量指数、结节直径比较无统计学差异(P>0.05),情况见表 1。
| 表 1 良恶性甲状腺结节患者一般资料比较 Comparison of general data in patients with benign and malignant thyroid nodules |
所有患者均取仰卧位,采用Philips Brilliance 64层螺旋CT机扫描范围从主动脉弓到下颌角,扫描参数为120 kV、50 mA、1.8 s/层、层厚2.5 mm、层距2.5 mm。平扫后行增强检查,采用造影剂跟踪扫描,通过高压注射器经肘静脉注射碘帕醇(300 mg I/mL)、速率3 mL/s,动脉期扫描结束后30 s开始静脉期扫描,监测阈值为100 HU。
1.2.2 颈部MRI检查所有患者均取仰卧位,采用美国GE公司1.5T Signa磁共振扫描仪,通过头颈联合表面线圈对颈部行自旋回波(spin echo, SE)的常规横断面、冠状面及矢状面的T1WI和T2WI扫描,扫描设置为层厚2.5 mm、矩阵256×256、视野(field of vision, FOV)220 mm×180 mm、横轴位SE T1WI[重复时间(repetition time, TR)600 ms/回波时间(echo time, TE)15 ms)]、快速自旋回波序列(fast spin echo, FSE)T2WI(TR440 ms/TE100 ms),必要时保持体位以3.5 mm层厚于T1WI横断和冠状面行增强扫描。
1.2.3 图像分析[4, 5](1) 阅片方法,CT、MRI均由同一组经验丰富(从事影像学诊断3年以上、取得相关资格证书)的医师进行阅片诊断,观察甲状腺结节形态、边界、大小、信号/密度、钙化、颈部淋巴结等影像学特征,最后得出诊断结果,意见不一时,由另一位同等资历医师参与诊断,最终结果遵从少数服从多数原则。(2)CT诊断标准,CT示囊内钙化性结节和囊内乳状头结节、甲状腺呈弥漫性肿大、肿瘤实体内具有细沙粒样钙化存在、肿瘤不规则低密度影、瘤体包膜连续性中断、肿瘤壁不规则且边界不清楚。(3)MRI诊断标准,MRI示肿瘤呈不规则形状且信号不均匀、边缘模糊不清楚、肿瘤周围低信号影并呈不完整包膜样出现、甲状腺周围组织出现浸润且淋巴结组织已转移、T2加权为高信号、T1加权信号为低信号或正常。
1.3 统计学方法不同方法对良恶性甲状腺结节的鉴别价值采用四格表法计算,敏感度=真恶性数/恶性数×100%,特异度=真良性数/良性数×100%,准确度=(真恶性数+真良性数)/总数×100%。采用SPSS 22.0软件处理,计数资料以(%)表示采用χ2检验,计量资料以(x±s)表示采用独立样本t检验,P < 0.05为差异有统计学意义。
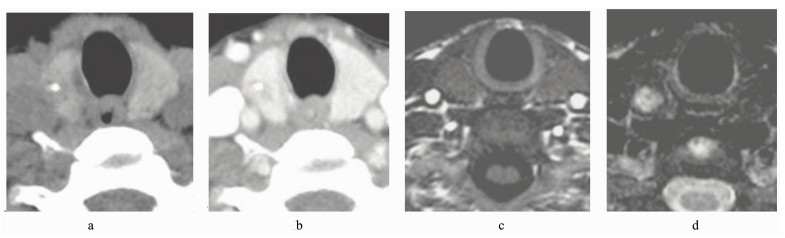
2 结果 2.1 甲状腺结节患者CT、MRI检查结果MRI总病灶、形态不规则、边界不清/毛糙、信号/密度不均检出率明显高于CT,MRI钙化灶检出率明显低于CT,差异有统计学意义(P < 0.05),CT、MRI淋巴结转移检出率比较,差异无统计学意义(P>0.05),见表 2。典型病例见图 1。
| 表 2 甲状腺结节患者CT、MRI检查结果比较(例/%) Comparison of CT and MRI findings in patients with thyroid nodules (case/%) |
|
图 1 甲状腺结节患者CT、MRI检查结果 女,52岁,病理结果显示右侧甲状腺乳头状癌;a为CT平扫、b为CT增强,示低密度、伴小钙化灶;c为MRI的T1WI、d为MRI的T2WI,示T1WI等信号、T2WI不均匀高信号、清晰显示结节边缘不明显、形态相对不规则,但钙化显示不清 CT and MRI findings of patients with thyroid nodules Female, 52 years old, pathological findings showed right papillary thyroid cancer; a was CT plain scan, b was CT enhancement, they were showed low density and small calcification; c was T1WI of MRI, d was T2WI of MRI, they were showed T1WI signal, heterogeneous high signal of T2WI, clearly showing the edge of nodules was not obvious, the shape of nodules was relatively irregular, but the calcification was unclear |
在鉴别良恶性甲状腺结节的敏感度、特异度、准确度中,CT为79.17%(38/48)、74.51%(76/102)、76.00%(114/150),MRI为83.33%(40/48)、80.39%(82/102)、81.33%(122/150),CT联合MRI为95.83%(46/48)、96.08%(98/102)、96.00%(144/150),CT联合MRI明显高于CT、MRI,差异有统计学意义(P < 0.05),见表 3、4。
| 表 3 不同方法鉴别良恶性甲状腺结节的效能分析(例) The differentiation of benign and malignant thyroid nodules by different methods (case) |
| 表 4 不同方法对良恶性甲状腺结节的鉴别价值比较(%) The differential value of different methods for benign and malignant thyroid nodules (%) |
甲状腺结节是常见的一种内分泌疾病,其良性病变多在体检中被检出、无特异性症状,且多数病变无需接受治疗,但其恶性病变发病率在人体内分泌性恶性肿瘤中居首位,多数为乳头状癌、滤泡状癌等分化型癌,采用根治性+淋巴结清扫手术治疗后预后较好[6]。而甲状腺结节恶性病变若未及早诊治,尤其是发生淋巴结转移后,易引起术后局部复发而导致预后欠佳,因此如何有效鉴别甲状腺结节的良恶性具有重要的临床意义[7]。目前,病理学检查是鉴别甲状腺结节良恶性的金标准,但其存在取材困难、有创、操作复杂、时间长等局限性,导致其难以广泛应用于甲状腺结节筛查中[8, 9]。而有研究显示,CT是诊断甲状腺疾病重要的影像学手段之一,具有很高的密度分辨力,尤其是多层螺旋CT技术的应用,有效提高了其空间分辨率,使其图像更清晰,有利于提供更准确的诊断依据[10, 11]。而MRI也是甲状腺疾病重要的诊断方法之一,具有多参数成像的特点,并可提供更多病灶及其与周围组织关系的信息,其诊断效能逐渐被认可[12, 13]。
本研究甲状腺结节患者CT、MRI检查结果显示,MRI总病灶、形态不规则、边界不清/毛糙、信号/密度不均检出率明显高于CT,MRI钙化灶检出率明显低于CT,CT、MRI淋巴结转移检出率比较无统计学差异,在鉴别良恶性甲状腺结节的敏感度、特异度、准确度中,CT为79.17%、74.51%、76.00%,MRI为83.33%、80.39%、81.33%,表明CT、MRI均能够作为鉴别良恶性甲状腺结节的重要方法,此结论与冯凯、Zander等[14, 15]的研究结果基本一致,并提示CT对钙化灶有较高的分辨能力,MRI对软组织及小病灶有较高的分辨能力。这可能是由于在恶性甲状腺结节发生发展中,因癌细胞已失去正常细胞的生长特性,其呈无规律、异常快速的生长状态,会对周围正常组织形成浸润而造成其坏死、钙化;因此其图像多为不规则形态、内部密度不均匀、不规则坏死区域、钙化等征象[11]。而良性甲状腺结节仍具有正常细胞规律的生长特性,其主要会推挤周围组织,故其图像多为低密度结节组织、边缘相对清晰、无坏死及钙化等征象[13]。此外,本研究通过CT联合MRI鉴别良恶性甲状腺结节时,其敏感度、特异度、准确度I为95.83%、96.08%、96.00%,CT联合MRI明显高于CT、MRI,表明CT联合MRI有效提高了良恶性甲状腺结节的鉴别价值。分析原因可能是单独CT检查中,虽能够较好地显示甲状腺结节钙化征象,但其对软组织及小病灶的分辨能力差,易导致误漏诊。而单独MRI检查虽能够较好地分辨软组织及小病灶,但其对甲状腺结节钙化征象显示模糊而易出现误漏诊。而本研究通过CT联合MRI检查时,可能有效弥补了各自的不足,从而能够为鉴别良恶性甲状腺结节提供更多、更准确的方式。因此,本研究认为在鉴别良恶性甲状腺结节中应进行CT联合MRI检查,而考虑CT具有操作简单、费用低等优势[16],故应优先对患者进行CT检查,对不能确诊者再行MRI检查,以提高临床鉴别准确性。
综上所述,CT、MRI可作为鉴别良恶性甲状腺结节的重要方法,CT对钙化灶有较高的分辨能力,MRI对软组织及小病灶有较高的分辨能力,CT联合MRI可有效提高其鉴别价值,值得临床推广。
| [1] |
杜芬, 胡珊, 梁梦, 程艳. 18F-FDGPET/CT显像在甲状腺偶发瘤良恶性诊断中的研究进展[J]. 国际放射医学核医学杂志, 2018, 42(3): 274-279. Du F, Hu S, Liang M, Cheng Y. Development in the diagnosis of benign and malignant thyroid incidentalomas by 18F-FDG PET/CTimaging[J]. International Journal of Radiation Medicine and Nuclear Medicine, 2018, 42(3): 274-279. DOI:10.3760/cma.j.issn.1673-4114.2018.03.015 |
| [2] |
高飞, 周辉, 王传彬, 李乃玉, 董江宁, 王婷婷, 魏欣扬, 曹锋. 结节性甲状腺肿的128层CT征象与病理表现的关系探讨[J]. 中国医学装备, 2018, 15(3): 66-70. Gao F, Zhou H, Wang C B, Li N Y, Dong J N, Wang T T, Wei X Y, Cao F. Discuss about the relationship of image features with 128-slices CT and pathological diagnosis on the NG[J]. China Medical Equipment, 2018, 15(3): 66-70. DOI:10.3969/J.ISSN.1672-8270.2018.03.018 |
| [3] |
段文飞, 姜文官, 李晶, 赵武, 宋瑶. B超、CT、MRI对甲状腺微小癌的诊断意义[J]. 中国医药导报, 2015, 12(25): 129-132. Duan W F, Jiang W G, Li J, Zhao W, Song Y. Diagnostic significance of B ultrasonic, CT, MRI on thyroid microcarcinoma[J]. China Medical Herald, 2015, 12(25): 129-132. |
| [4] |
Kim D W Jung S J, Baek H J, e t, a l. Computed tomography features of benign and malignant solid thyroid nodules[J]. Acta Radiologica:Diagnosis, 2015, 56(10): 1196-1202. DOI:10.1177/0284185114552216 |
| [5] |
Lu Y, Hatzoglou V, Banerjee S, Stambuk H E, Gonen M, Shankaranarayanan A, Mazaheri Y, Deasy J O, Shaha A R, Tuttle R M, Shukla-Dave A. Repeatability investigation of reduced field-of-view diffusion-weighted magnetic resonance imaging on thyroid glands[J]. Journal of Computer Assisted Tomography, 2015, 39(3): 334-9. |
| [6] |
刘建辉, 邓静. 甲状腺结节CT及MRI诊断临床探讨[J]. 中国继续医学教育, 2017, 9(10): 73-74. Liu J H, Deng J. Discussion on CT and MRI diagnosis of thyroid nodules[J]. China Continuing Medical Education, 2017, 9(10): 73-74. DOI:10.3969/j.issn.1674-9308.2017.10.037 |
| [7] |
Lee M, Lee Y K, Jeon T J, Park C S, Ryu Y H. 1311 Uptake in intraosseous hemangioma of the skull:Mimicking a bone metastasis in thyroid cancer[J]. Clinical Nuclear Medicine, 2014, 39(11): 990-992. DOI:10.1097/RLU.0000000000000467 |
| [8] |
许定华, 夏俊, 陈金凤, 罗树存, 罗泽斌. 甲状腺结节CT及病理分析[J]. 现代医用影像学, 2016, 25(6): 996-999. Xu D H, Xia J, Chen J F, Luo S C, Luo Z B. The CT and pathological analysis of thyroid nodules[J]. Modern Medical Imagelogy, 2016, 25(6): 996-999. |
| [9] |
Kim K S, Kim D W, Sung J Y. Detection of thyroid pyramidal lobe by ultrasound versus computed tomography:a single-center study[J]. Journal of Computer Assisted Tomography, 2014, 38(3): 464-468. DOI:10.1097/RCT.0000000000000054 |
| [10] |
姚强, 陈孙斌, 符传刚, 陈春妃. 结节性甲状腺肿合并甲状腺癌的超声及CT诊断分析[J]. 中国CT和MRI杂志, 2016, 14(6): 22-24. Yao Q, Chen S B, Fu C G, Chen C F. Analysis of ultrasound and CT diagnosis of nodular goiter with thyroid cancer[J]. Chinese Journal of CT and MRI, 2016, 14(6): 22-24. DOI:10.3969/j.issn.1672-5131.2016.06.008 |
| [11] |
Ovchinnikov V A, Ovchinnikov E A. Computed tomography in diagnostics of extravasal influence of thyroid nodules[J]. Khirurgiia(Mosk), 2016(1): 20-24. |
| [12] |
张书卿, 张裘, 张博, 洪亮, 龙学颖. MRI在甲状腺肿瘤的肿块定位和良恶性判断中的应用研究[J]. 现代生物医学进展, 2015, 15(10): 1885-1887. Zhang S Q, Zhang Q, Zhang B, Hong L, Long X Y. Research on the application of MRI for the mass orientation and differentiation diagnosis of thyroid tumor[J]. Progress in Modern Biomedicine, 2015, 15(10): 1885-1887. |
| [13] |
Kasbekar A V, Swords C, Attlmayr B, Kulkarni T, Swift A C. Sinonasal papilloma:what influences the decision to request a magnetic resonance imaging scan?[J]. Journal of Laryngology and Otology, 2018, 132(7): 584-590. DOI:10.1017/S0022215118000804 |
| [14] |
冯凯, 童进, 刘国保. 甲状腺结节CT及MRI诊断效果探究[J]. 中国医疗器械信息, 2017, 23(19): 65-66. Feng K, Tong J, Liu G B. Study on CT and MRI diagnosis of thyroid nodules[J]. China Medical Devices Information, 2017, 23(19): 65-66. DOI:10.3969/j.issn.1006-6586.2017.19.026 |
| [15] |
Zander D A, Smoker W R. Imaging of ectopic thyroid tissue and thyroglossal duct cysts[J]. Radiographics, 2014, 34(1): 37-50. DOI:10.1148/rg.341135055 |
| [16] |
Xu F, Shao Z, Yang G, Gu A, Jiang M, Pan Y, Ma Y. The value of scintigraphy, computed tomography, magnetic resonance imaging, and single-photon emission computed tomography/computed tomography for the diagnosis of ectopic thyroid in the head and neck:A STROBE-compliant retrospective study[J]. Medicine (Baltimore), 2018, 97(13): e0239. DOI:10.1097/MD.0000000000010239 |




