凶险性前置胎盘是指既往有剖宫产史,且此次妊娠为前置胎盘,胎盘附着在原子宫切口瘢痕部位,部分患者伴有胎盘植入,是引起产前、产时与产后大出血的重要原因[1]。既往研究表明[2]:凶险性前置胎盘病因复杂,普遍认为与不孕治疗史、剖宫产史及孕妇年龄有关,会增加休克、弥漫性血管内凝(DIC)等并发症发生率。组织病理学中,将胎盘植入分为粘连性胎盘、植入性胎盘与穿透性胎盘3种,而其中穿透性凶险性前置胎盘最为严重,是发生率较高的妊娠期并发症[3, 4],目前,临床上对于穿透性凶险性前置胎盘以剖宫产终止妊娠为主,但是患者分娩过程中如何控制出血缺乏统一的标准。子宫动脉栓塞术属于一种微创治疗方法,能暂时阻断子宫血液循环,且栓塞材料以明胶海绵颗粒为主,具有安全、止血迅速、保留子宫等优点[5, 6]。本研究选择我院收治的45例穿透性凶险性前置胎盘患者作为研究对象,探讨DSA引导下双侧子宫动脉栓塞术治疗穿透性凶险性前置胎盘的效果及对患者临床结局的影响。
1 资料与方法 1.1 临床资料选择2017年12月~2019年7月我院收治的穿透性凶险性前置胎盘患者45例,术前与孕妇及家属充分沟通子宫动脉栓塞术的利弊,依据知情同意原则,由孕妇及家属自愿选择是否行子宫动脉栓塞术,并签署知情同意书。其中,选择行子宫动脉栓塞术的25例患者作为观察组,年龄28~36岁,平均(33.41±1.63)岁;孕周34~30周,平均(35.81±2.21)周;孕次1~6次,平均(2.96±0.58)次;非前壁胎盘14例,前壁胎盘11例。未选择子宫动脉栓塞术的20例患者作为对照组,年龄30~35岁,平均(33.12±1.59)岁;孕周34~39周,平均(35.74±2.15)周;孕次1~5次,平均(2.91±0.53)次;非前壁胎盘12例,前壁胎盘8例。本研究经医院医学伦理委员会批准,两组患者一般资料比较差异均无统计学意义(P>0.05),具有可比性。
1.2 纳入和排除标准纳入标准:(1)均符合前置胎盘诊断标准[7],患者均为穿透性凶险性前置胎盘;(2)均经彩超、磁共振确诊,且胎盘植入已经通过术中、术后病理确诊;(3)符合DSA引导下双侧子宫动脉栓塞术治疗适应证,且患者均可耐受;(4)意识清楚,能与医生进行沟通、交流。排除标准:(1)合并精神异常、认知功能障碍或入院资料不全者;(2)合并凝血功能异常、恶性肿瘤或伴有严重肝肾异常者;(3)合并引产、内科疾病或具有产后出血史者。
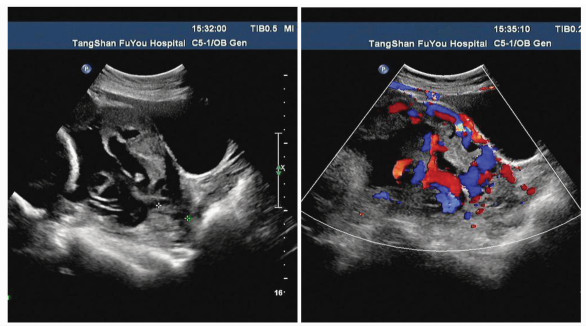
1.3 治疗方法两组术前均完善血常规、心电图、肝肾功、电解质、凝血功能等常规检查,应用彩色多普勒超声血流显像观察胎盘后间隙及子宫肌层血流情况(图 1),判断有无胎盘植入,并了解胎儿宫内情况。
|
图 1 穿透性凶险性前置胎盘超声图像(三维超声显示胎盘内血管走行分支杂乱) Penetrating and dangerous ultrasound image of placenta previa (three-dimensional ultrasound can show the disordered branches of blood vessels in placenta) |
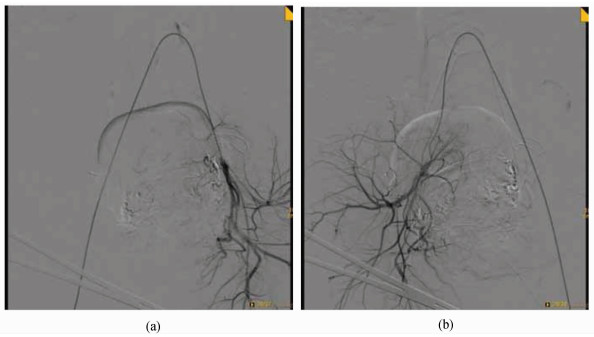
对照组患者给予常规剖宫产手术治疗:产妇均给予剖宫产终止妊娠,分娩后完成胎盘处理,术中结合患者情况完成子宫按摩,常规给予宫缩剂,积极采取多种措施帮助患者止血,必要时可切除子宫[8]。观察组患者在DSA引导下行双侧子宫动脉栓塞术治疗:取平卧位姿势,常规进行消毒、铺巾,患者均给予硬膜外麻醉,待麻醉生效后以右下肢股动脉入路,借助Seldinger’s穿刺技术完成右侧股动脉穿刺,并置入5F血管鞘、子宫动脉造影。上述操作成功后将患者置于手术台上,进行剖宫产手术。术中再次评估患者出血情况,将子宫下段切开打开,对于大量血涌出者,胎盘植入较为严重,尽可能避开胎盘作手术切口,待胎儿娩出后暂不处理胎盘,完成切口边缘钳夹;给予患者宫腔内纱布填塞,完成暂时性压迫止血,在DSA监视下选择导管并到达左侧子宫动脉,完成造影手术,进一步确定子宫动脉的走形、病灶血供情况(对侧以同样发放处理);根据检查结果选择明胶海绵颗粒1~2 mm,对于合并子宫动静脉瘘患者给予明胶海绵处理,再次给予SA检查,栓塞成功后拔出导管与鞘(图 2),并给予右下肢穿刺止血,常规绷带加压包扎止血。手术过程中逐步剥离、清除胎盘,完成肌层缺损区域修补、缝合子宫;对于子宫保留困难或出血量较大者行子宫切除手术,术后7天对患者效果进行评估。
|
图 2 子宫动脉栓塞术后造影图像 (a)使用明胶海绵颗粒栓塞左侧子宫动脉后, 行左侧髂内动脉造影示子宫动脉栓塞良好; (b)使用明胶海绵颗粒栓塞右侧子宫动脉后, 行右侧髂内动脉造影示子宫动脉栓塞良好 Contrast image after uterine artery embolization (a) After embolization of left uterine artery with gelatin sponge granules, left internal iliac artery angiography showed that uterine artery embolization was good; (b) after embolization of right uterine artery with gelatin sponge granules, right internal iliac artery angiography showed that uterine artery embolization was good |
(1) 手术指标及新生儿Agpar评分:记录两组失血量、红细胞输血量、冷沉淀输血量、住院时间及新生儿1 min Agpar评分[9]; (2)母婴结局:记录两组新生儿肺炎、新生儿呼吸窘迫综合征、新生儿窒息及新生儿高胆红素血症发生率; (3)并发症发生率:记录两组子宫切除、产后出血、产褥感染、失血性休克与DIC发生率。
1.5 统计学分析采用SPSS 18.0软件处理,计数资料行χ2检验,采用n(%)表示,计量资料行t检验,采用(x±s)表示,P < 0.05差异有统计学意义。
2 结果 2.1 两组手术指标及新生儿Agpar评分比较观察组失血量、红细胞输血量、冷沉淀输血量、住院时间,少(短)于对照组,新生儿1 min Agpar评分高于对照组,差异有统计学意义(P < 0.05),见表 1。
| 表 1 两组手术指标及新生儿Agpar评分比较(分,x±s) Comparison of surgical indicators and neonatal Agpar scores between two groups (score, x±s) |
观察组新生儿肺炎、新生儿呼吸窘迫综合征、新生儿窒息及新生儿高胆红素血症发生率均低于对照组,差异有统计学意义(P < 0.05),见表 2。
| 表 2 两组母婴结局比较[n(%)] Comparison of maternal and infant outcomes between the two groups [n(%)] |
两组产褥感染率无统计学意义(P>0.05),观察组子宫切除、产后出血、失血性休克和DIC发生率均低于对照组,差异有统计学意义(P < 0.05),见表 3。
| 表 3 两组并发症比较[n(%)] Comparisons between the two groups [n(%)] |
胎盘植入是妊娠期常见的并发症,尤其是穿透性胎盘,胎盘入侵子宫肌层并达到浆膜层,部分患者甚至侵入膀胱、直肠等邻近组织,具有发生率高、死亡率高等特点[10]。剖宫产是穿透性凶险性前置胎盘患者常用的治疗方法,虽然能满足分娩需要,但是远期预后较差,患者子宫切除率较高,难以满足年轻产妇治疗需要[11]。
近年来,DSA引导下双侧子宫动脉栓塞术在穿透性凶险性前置胎盘患者中得到应用,且效果理想。本研究中,观察组失血量、红细胞输血量、冷沉淀输血量、住院时间,少(短)于对照组(P < 0.05),说明DSA引导下双侧子宫动脉栓塞术能减少穿透性凶险性前置胎盘患者输血量、缩短住院时间,利于患者恢复。介入治疗是穿透性凶险性前置胎盘患者首选治疗方法,最早于1979年首次提出,且随着放射性血管介入技术的发展,该治疗方法得到推广。目前,临床上血管介入治疗方法包括球囊阻塞术、动脉栓塞术两种[12]。但是,由于球囊阻塞术并发症发生率较高,手术治疗适应证较窄,导致该方法并未得到推广[13]。而动脉栓塞术在穿透性凶险性前置胎盘患者中发挥了重要作用,能暂时阻断子宫血液循环,并且能在盆腔血管脏支、脏支与壁支之间建立吻合,能为子宫提供足够的血供。同时,子宫动脉栓塞术具有微创、止血迅速、安全及保留子宫等优点,能获得较高的出血成功率[14]。本研究中,观察组新生儿1 min Agpar评分高于对照组(P < 0.05), 新生儿肺炎、新生儿呼吸窘迫综合征、新生儿窒息及新生儿高胆红素血症发生率均低于对照组(P < 0.05),说明DSA引导下双侧子宫动脉栓塞术用于穿透性凶险性前置胎盘患者的治疗能获得良好的母婴结局。
既往研究表明[15]:放射血管介入最早用于产后出血,对于穿透性凶险性前置胎盘患者,出血相对凶猛, 因此,子宫动脉栓塞时机较为重要。国内学者研究发现,患者发生大出血后进行介入治疗,出血量在1000~4000 mL,虽然能降低死亡率、子宫切除率,但是患者常伴有休克、DIC等症状。因此,患者行剖宫产时应尽早给予介入栓塞治疗,不断完善外科操作及介入治疗方法,优化患者介入治疗时机,避免胎儿暴露于DSA下。待胎儿娩出后对胎盘边缘进行钳夹,完成双侧髂内动脉或子宫动脉栓塞术,减少子宫出血量,及时清除粘连或植入的胎盘组织,栓塞、阻断子宫供血,降低术后并发症发生率。本研究中,两组产褥感染率无统计学意义(P>0.05),观察组子宫切除、产后出血、失血性休克与DIC发生率,低于对照组(P < 0.05),说明DSA引导下双侧子宫动脉栓塞术治疗穿透性凶险性前置胎盘具有较高的安全性,有助于提高患者耐受性。
综上所述,DSA引导下双侧子宫动脉栓塞术治疗穿透性凶险性前置胎盘的效果确切,可明显减少患者术中出血量及术后并发症,降低手术风险,改善临床结局,且微创、安全,值得临床推广应用。
| [1] |
王慰敏, 马强, 刘睿, 秦皓, 田红燕, 白桂芹. 嵌合杂交手术系统在凶险性前置胎盘中的疗效评价[J]. 中国妇幼健康研究, 2017, 28(10): 1232-1235. Wang W M, Ma Q, Liu R, Qin H, Tian H Y, Bai G Q. Evaluation of the efficacy of chimeric hybridization system in dangerous placenta previa[J]. China Maternal and Child Health Study, 2017, 28(10): 1232-1235. DOI:10.3969/j.issn.1673-5293.2017.10.023 |
| [2] |
李钦, 张雪梅, 赵建林, 熊希, 李海营, 漆洪波. 剖宫产术中不同腹主动脉球囊阻断时机对凶险性前置胎盘母婴结局的影响[J]. 实用妇产科杂志, 2018, 34(5): 63-66. Li Q, Zhang X M, Zhao J L, Xiong X, Li H Y, Qi H B. The effect of different timing of abdominal aortic balloon occlusion on the maternal and infant outcomes of dangerous placenta previa during cesarean section[J]. Journal of Practical Gynecology and Obstetrics, 2018, 34(5): 63-66. |
| [3] |
Wang Y, Huang X. Sepsis after uterine artery embolization-assisted termination of pregnancy with complete placenta previa:a case report[J]. The Journal of International Medical Research, 2017, 46(1): 546-550. |
| [4] |
阚红莉. 数字减影血管造影下选择性子宫动脉栓塞术治疗子宫肌瘤的疗效及对VEGF、MMP-2和TNF-α的影响[J]. 中国妇幼保健, 2017, 32(20): 5132-5135. Kan H L. The efficacy of selective uterine artery embolization under digital subtraction angiography in the treatment of uterine leiomyoma and its effects on vascular endothelial growth factor, MMP-2 and TNF-alpha[J]. Maternal and Child Health Care of China, 2017, 32(20): 5132-5135. |
| [5] |
周巾, 郭艳萍, 季淑英. 髂内动脉预置球囊、双侧子宫动脉栓塞对凶险性前置胎盘患者剖宫产术中出血的预防效果比较[J]. 山东医药, 2017, 57(39): 56-58. Zhou J, Guo Y P, Ji S Y. Pre-balloon of internal iliac artery and bilateral uterine artery embolization for prevention of bleeding during cesarean section in patients with dangerous placenta previa[J]. Shandong Medicine, 2017, 57(39): 56-58. DOI:10.3969/j.issn.1002-266X.2017.39.017 |
| [6] |
刘丽娟, 曹淑新, 桑雪梅, 李宇鑫, 姜海英. 子宫动脉栓塞术在穿透性凶险性前置胎盘中的临床应用研究[J]. 现代生物医学进展, 2017, 17(6): 1135-1137. Liu L J, Cao S X, Sang X M, Li Y X, Jiang H Y. Clinical application of uterine artery embolization in penetrating and dangerous placenta previa[J]. Advances in Modern Biomedicine, 2017, 17(6): 1135-1137. |
| [7] |
钱敏, 单楠, 漆洪波. 腹主动脉球囊阻断术联合子宫动脉栓塞术对凶险性前置胎盘的治疗效果[J]. 西部医学, 2018, 30(12): 48-52. Qian M, Shan N, Qi H B. The therapeutic effect of abdominal aortic balloon occlusion combined with uterine artery embolization on dangerous placenta previa[J]. Western Medicine, 2018, 30(12): 48-52. |
| [8] |
马俊, 陈葵喜, 程珊, 吴间开, 颜为红. 子宫动脉栓塞术治疗凶险性前置胎盘的应用效果评价[J]. 中国计划生育和妇产科, 2017, 9(11): 43-46. Ma J, Chen K X, Cheng S, Wu J K, Yan W H. Evaluation of the effect of uterine artery embolization in the treatment of dangerous placenta previa[J]. Chinese Journal of Family Planning & Gynecotokology, 2017, 9(11): 43-46. DOI:10.3969/j.issn.1674-4020.2017.11.11 |
| [9] |
杨玉侠, 张颖, 季淑英. 子宫动脉栓塞术在凶险性前置胎盘伴胎盘植入中的应用效果[J]. 中国煤炭工业医学杂志, 2016, 19(1): 35-38. Yang Y X, Zhang Y, Ji S Y. Uterine artery embolization in the treatment of dangerous placenta previa with placenta implantation[J]. Chinese Journal of Coal Industry Medicine, 2016, 19(1): 35-38. |
| [10] |
张宏. Forgarty导管腹主动脉阻断联合子宫动脉栓塞术在凶险性前置胎盘剖宫产术中的临床研究[J]. 中南医学科学杂志, 2018, 46(3): 90-93. Zhang H. Clinical study of Forgarty catheter abdominal aorta occlusion combined with uterine artery embolization in caesarean section with dangerous placenta previa[J]. Journal of Central South Medical Science, 2018, 46(3): 90-93. |
| [11] |
Fan Y, Gong X, Wang N, Mu K, Feng L, Qiao F, Chen S, Zeng W, Liu H, Wu Y, Zhou Q, Tian Y, Li Q, Yang M, Li F, He M, Beejadhursing R, Deng D. A prospective observational study evaluating the efficacy of prophylactic internal iliac artery balloon catheterization in the management of placenta previa-accreta:a strobe compliant article[J]. Medicine (Baltimore), 2017, 96(45): e8276. DOI:10.1097/MD.0000000000008276 |
| [12] |
马颖, 郭咏梅, 陈建虹, 刘春华. 两种不同止血方式对凶险性前置胎盘患者剖宫产术中出血及预后的影响[J]. 中国妇幼健康研究, 2017, 28(10): 1229-1231. Ma Y, Guo Y M, Chen J H, Liu C H. The effects of two different hemostasis methods on bleeding and prognosis in caesarean section of patients with dangerous placenta previa[J]. China Maternal and Child Health Research, 2017, 28(10): 1229-1231. DOI:10.3969/j.issn.1673-5293.2017.10.022 |
| [13] |
黄智勇, 江琴, 李昭辉, 郭伟昌, 彭翼. Forgarty导管腹主动脉阻断联合子宫动脉栓塞在凶险型前置胎盘患者剖宫产术中的应用[J]. 临床误诊误治, 2017, 30(7): 66-70. Huang Z Y, Jiang Q, Li Z H, Guo W C, Peng Y. Application of Forgarty catheter abdominal aorta occlusion combined with uterine artery embolization in caesarean section for patients with dangerous placenta previa[J]. Clinical Misdiagnosis and Mistreatment, 2017, 30(7): 66-70. DOI:10.3969/j.issn.1002-3429.2017.07.021 |
| [14] |
郭琼. 子宫动脉下行支结扎联合子宫下段压迫缩窄缝合术在凶险性前置胎盘所致产后出血中的应用[J]. 实用临床医药杂志, 2017, 21(3): 85-88. Guo Q. Application of ligation of descending uterine artery branch combined with compression and constriction suture of lower uterine segment in the treatment of postpartum hemorrhage caused by dangerous placenta previa[J]. Journal of Practical Clinical Medicine, 2017, 21(3): 85-88. |
| [15] |
范文龙, 杨正强, 夏金国, 周卫忠, 施海彬. 腹主动脉球囊阻断与子宫动脉预置导管栓塞辅助凶险性前置胎盘剖宫产效果比较[J]. 介入放射学杂志, 2018, 27(10): 24-27. Fan W L, Yang Z Q, Xia J G, Zhou W Z, Shi H B. Comparison of the effect of abdominal aortic balloon occlusion and uterine artery pre-catheter embolization in assisting dangerous placenta previa cesarean section[J]. Journal of Interventional Radiology, 2018, 27(10): 24-27. |




