2. 邢台市第三医院 检验科, 河北 邢台 054000;
3. 邢台市第三医院 产科, 河北 邢台 054000
2. Department of Laboratory, Xingtai Third Hospital, Xingtai 054000, Hebei, P. R. China;
3. Department of Obstetrics, Xingtai Third Hospital, Xingtai 054000, Hebei, P. R. China
高危妊娠是指在妊娠期间存在某种致病因素和并发症,会对孕妇、胎儿及新生儿构成危险并可能导致不良妊娠结局,如胎儿宫内窘迫、胎儿生长受限、新生儿窒息等[1]。近年来,随着二胎政策的开放和晚婚晚育人数的增加,高危妊娠人数也逐年上升,如何早预防、早发现、早治疗以改善高危妊娠引起的不良妊娠结局,是产科面临的重大问题[2]。彩色多普勒超声(CDFI)因具有安全、无创、快捷、敏感性较高、可重复性好、价格低廉等优势,广泛应用于产科领域。CDFI与常规二维超声相结合,可显示血流的分布情况,联合频谱多普勒,可定量测量血流速度及相应比值,更好地反映血管中血流的分布及通过情况[3]。本研究通过超声监测高危妊娠晚期胎儿脐动脉、大脑中动脉血流动力学多普勒参数的变化情况,为判定胎儿宫内状况、指导临床治疗、预测不良妊娠结局及选择最佳分娩时机提供了客观依据。
1 资料与方法 1.1 一般资料选取2018年1月~2019年1月于我院行产前检查的高危妊娠晚期孕妇100例作为观察组,年龄22~40岁,平均(32.21±2.90)岁;孕周34~36周,平均(34.93±0.29)周;妊娠合并症:妊娠期高血压疾病28例、妊娠期糖尿病20例、妊娠期甲状腺功能减退15例、羊水过多13例、羊水过少10例、妊娠期贫血8例、妊娠期肝内胆汁淤积6例。另选取同期正常妊娠孕妇100例作为对照组,孕妇年龄23~39岁,平均(32.50±2.31)岁;孕周34~36周,平均(35.01±0.30)周;妊娠无合并症。本研究经医院医学伦理委员会批准,患者及家属均知情同意。两组孕妇一般资料比较差异均无统计学意义(P>0.05),具有可比性。
1.2 纳入及排除标准[4]纳入标准:(1)均符合《临床诊疗指南·妇产科学分册》中高危妊娠的诊断标准;(2)病例资料完整,均在我院定期产检并住院分娩;(3)孕周34~36周,宫内单活胎;(4)孕期无特殊用药史,胎儿无先天发育畸形;(5)不伴脐带及胎盘异常。
排除标准:(1)超声提示胎儿先天发育异常,或伴有脐带及胎盘异常;(2)超声检查显示双胎或多胎;(3)存在严重心、肝、肾等疾病及血液系统疾病;(4)合并有生殖器畸形或生殖器疾病等;(5)下腹部及盆腔手术史。
1.3 方法 1.3.1 仪器与设备选用美国GE voluson E8彩色多普勒超声诊断仪,探头:C1-5-D凸阵探头,探头频率为3.5~5 mHz。
1.3.2 检查方法二维超声检查:患者仰卧于检查床上,充分暴露孕肚,按照中晚孕检查流程进行检查,测量胎儿的双顶径、头围、腹围、股骨等,检查胎盘、羊水、脐带、胎心等情况有无异常。探查脐动脉:先探到胎盘脐带连接口和胎儿腹部脐带入口,在羊水中找出游离的脐带,结合孕妇情况调节探头的位置、角度,选择血流充盈、信号较好的动脉频谱完成取样,取样线保证与血流方向一致或偏角30°以内,采集至少5个连续稳定波形冻结图谱,测量胎儿脐动脉搏动指数(PI)、阻力指数(RI)、收缩期末峰值(PSV)、舒张期末峰值(EDV),并计算PSV/EDV(S/D)值。探查胎儿大脑中动脉:二维图像显示胎儿横切面,在显示大脑脚的切面上加彩色多普勒即可显示基底动脉环,大致垂直于大脑中线彩色血流即为大脑中动脉,在近端1/2部位取样,取样线保证与血流方向平行,不宜超过30°夹角,采集至少5个连续稳定波形冻结图谱,测量胎儿大脑中动脉PI、RI及S/D值。
1.4 观察指标统计高危妊娠组和对照组孕妇的妊娠结局;比较高危妊娠组和对照组胎儿脐动脉、大脑中动脉血流参数PI、RI及S/D值;比较高危妊娠结局正常组和高危妊娠结局异常组胎儿脐动脉、大脑中动脉血流参数PI、RI及S/D值。
1.5 统计学方法采用SPSS 22.0软件进行数据处理,计量资料采用(x±s)表示,行t检验;计数资料采用[n(%)]表示,行χ2检验,P < 0.05为差异有统计学意义。
2 结果 2.1 两组孕妇妊娠结局比较高危妊娠组中妊娠结局正常58例,妊娠结局异常42例(包括新生儿窒息6例、FGR 7例、早产11例、胎儿宫内窘迫18例),发生率为42.00%;对照组中妊娠结局正常95例,妊娠结局异常5例(包括早产1例、FGR 1例、胎儿宫内窘迫3例),发生率为5.00%。高危妊娠组妊娠结局异常率明显高于对照组,差异有统计学意义(P < 0.05)。
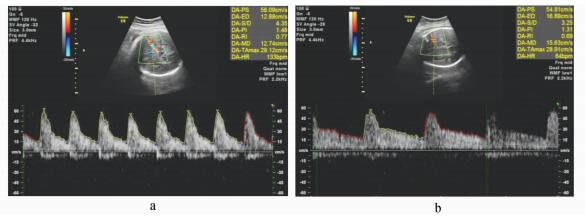
2.2 两组胎儿脐动脉、大脑中动脉血流参数比较高危妊娠组胎儿脐动脉血流参数PI、RI及S/D值均明显高于对照组,差异有统计学意义(P < 0.05);高危妊娠组胎儿大脑中动脉血流参数PI、RI及S/D值均明显低于对照组,差异有统计学意义(P < 0.05),详见表 1。图 1和图 2为胎儿脐动脉与大脑中动脉的多普勒频谱图。
| 表 1 两组胎儿脐动脉、大脑中动脉血流参数比较(x±s) |

|
图 1 胎儿脐动脉多普勒频谱图 a.对照组胎儿脐动脉多普勒频谱图;b.高危妊娠组典型胎儿脐动脉多普勒频谱图 |
|
图 2 胎儿大脑中动脉多普勒频谱图 a.对照组胎儿大脑中动脉多普勒频谱图;b.高危妊娠组典型胎儿大脑中动脉多普勒频谱图 |
高危妊娠结局异常组胎儿脐动脉血流参数PI、RI及S/D值均明显高于妊娠结局正常组,差异有统计学意义(P < 0.05);高危妊娠结局异常组胎儿大脑中动脉血流参数PI、RI及S/D值均明显低于妊娠结局正常组,差异有统计学意义(P < 0.05),详见表 2。
| 表 2 高危妊娠结局正常组和异常组胎儿脐动脉、大脑中动脉血流参数比较(x±s) |
在产科临床中,产前检查为预测胎儿健康的主要方式,可有效诊断胎儿心率、胎儿缺氧及各种不良妊娠情况[5]。我国二胎政策开放后,孕产妇数量逐年上升,高危妊娠具有较高的风险性,危及产妇及胎儿的生命安全,部分产妇在分娩时会出现难产、新生儿窒息、死胎等情况[6]。二维超声可以对胎儿生长发育情况、胎心率、胎动、羊水、脐带等指标进行直接观察,具有安全、无创、快捷、敏感性较高、可重复性好、价格低廉等优势,广泛应用于产科临床诊疗中[7]。通过监测高危妊娠晚期胎儿脐动脉、大脑中动脉血流动力学多普勒参数PI、RI、S/D值,可为全面评估胎儿宫内状况及预测不良妊娠结局提供依据[8]。
脐动脉的血流变化可以反映胎儿-胎盘循环的血流动力学状态,是目前临床上观察胎儿血流动力学变化最常用的血管[9]。正常情况下,随妊娠进展,胎盘逐渐发育成熟,三级绒毛逐渐成熟,胎盘中的微血管数量增多、管径增粗,胎盘血流增多,PI、RI、S/D逐渐下降[10]。本研究结果显示,高危妊娠组胎儿脐动脉血流参数PI、RI及S/D值均明显高于对照组(P < 0.05),且高危妊娠结局异常组胎儿脐动脉血流参数PI、RI及S/D值均明显高于妊娠结局正常组(P < 0.05),表明胎儿脐动脉血流多普勒参数变化是判断胎儿宫内状况、预测不良妊娠结局的重要指标。妊娠晚期胎盘的发育趋于成熟,其中绒毛的毛细血管会呈现扩大状态,到产前绒毛间隙会增大到临界值,胎盘的局部血流量增大,降低了动脉血管的阻力,从而增加了胎盘血流量,因此胎儿脐动脉血管阻力降低,以确保胎儿的正常生产发育,保证充足的血流供应[11, 12]。高危妊娠时由于如妊高症等因素,胎盘的绒毛血管极有可能出现水肿、痉挛、内皮增生及梗塞等现象,导致动脉管腔狭窄,绒毛的动脉血管总横截面积降低,导致胎儿与胎盘之间的血液循环阻力上升,使胎儿脐动脉血流参数出现不同程度上升[13, 14]。因此,监测胎儿脐动脉血流多普勒参数变化可直接反映胎盘供血情况、胎盘循环功能及胎儿预后,对评估胎儿宫内情况及预测不良妊娠结局均具有一定的临床意义。
大脑中动脉是颈内动脉的主要分支,供应大脑半球所需的80%血液,也是超声下最容易监测的大脑血管,其血流参数可用于评估胎儿颅脑血液循环状态和胎儿缺氧的严重程度[15]。正常情况下随着妊娠进展,胎儿脑血管逐渐发育,管径增粗、阻力减小,脑血流量增加以满足大脑的需要[16]。当胎盘相对缺氧时,血液重新分配,胎儿颅脑动脉管腔阻力降低,血液流量及流速增加,外周血管的血流量降低,阻力上升,呈现为“脑保护效应”[17]。本研究结果显示,高危妊娠组胎儿大脑中动脉血流参数PI、RI及S/D值均明显低于对照组(P < 0.05),且高危妊娠结局异常组胎儿大脑中动脉血流参数PI、RI及S/D值均明显低于妊娠结局正常组(P < 0.05),表明胎儿大脑中动脉血流参数变化可能是高危妊娠时胎儿-胎盘血液循环不足,胎儿宫内缺氧引发脑保护效应所致[18],是判断胎儿宫内状况、预测不良妊娠结局的重要指标。因此,监测胎儿大脑中动脉血流参数变化可直接反映胎儿大脑循环的发育状态。
综上所述,高危妊娠晚期胎儿脐动脉、大脑中动脉血流多普勒参数变化,对判断胎儿宫内状况、预测不良妊娠结局均具有一定的临床意义,值得临床推广应用。
| [1] |
曹晶晶. 高危妊娠产妇的高危因素及治疗措施探讨[J]. 吉林医学, 2018, 39(1): 161-163. Cao J J. High risk factors and treatment measures of high risk pregnant women[J]. Jilin Medical Journal, 2018, 39(1): 161-163. DOI:10.3969/j.issn.1004-0412.2018.01.065 |
| [2] |
姚秉彝, 唐龙英, 仲伟国, 等. 高危妊娠管理对妊娠结局的影响[J]. 中国妇幼保健, 2020, 35(3): 403-405. Yao B Y, Tang L Y, Zhong W G, et al. The influence of high risk pregnancy management on pregnancy outcome[J]. Mate-rnal and Child Health Care of China, 2020, 35(3): 403-405. |
| [3] |
贾丽. 子宫动脉和脐动脉多普勒超声技术对高危妊娠结局预测的临床应用价值[J]. 中国临床医生杂志, 2017, 45(5): 89-91. Jia L. The clinical application value of uterine artery and umbilical artery Doppler ultrasound in predicting the outcome of high-risk pregnancy[J]. Chinese Journal of Clinicians, 2017, 45(5): 89-91. DOI:10.3969/j.issn.2095-8552.2017.05.033 |
| [4] |
谢幸, 孔北华, 段涛. 妇产科学[M]. 第9版. 北京: 人民卫生出版社, 2018: 375-376. Xie X, Kong B H, Duan T. Obstetrics and Gynecology[M]. 9th Edition. Beijing: People's Health Publishing House, 2018: 375-376. |
| [5] |
陈江红, 王娜, 黄乃磊. 脐动脉和胎儿大脑中动脉血流频谱预测新生儿缺血缺氧性脑病的价值[J]. 广东医学, 2017, 38(11): 1707-1710. Chen J H, Wang N, Huang N L. The value of umbilical artery and fetal middle cerebral artery blood flow spectrum in predicting neonatal hypoxic-ischemic encephalopathy[J]. Guangdong Medical Journal, 2017, 38(11): 1707-1710. DOI:10.3969/j.issn.1001-9448.2017.11.022 |
| [6] |
刘银梅, 许丽梅. 彩超检测妊娠中晚期子宫动脉血流频谱在妊娠高血压综合征预测中的应用价值[J]. 中国妇幼保健, 2017, 32(2): 414-416. Liu Y M, Xu L M. The application value of color Doppler ultrasound in the prediction of pregnancy induced hypertension[J]. China Maternal and Child Health Care, 2017, 32(2): 414-416. |
| [7] |
陈树寰, 吴育杰, 刘春荣, 等. 妊娠晚期孕妇体位对彩色多普勒超声检测胎儿脐动脉和大脑中动脉血流影响[J]. 临床误诊误治, 2018, 276(8): 33-37. Chen S H, Wu Y J, Liu C R, et al. The influence of the position of pregnant women in late pregnancy on the detection of fetal umbilical artery and middle cerebral artery blood flow by color Doppler ultrasound[J]. Clinical Misdiagnosis and Mistreatment, 2018, 276(8): 33-37. |
| [8] |
张宇鹏, 于金华, 王新, 等. 超声检测妊娠期高血压孕妇胎儿血流动力学变化与妊娠结局的相关性分析[J]. 医学影像学杂志, 2018, 28(2): 308-312. Zhang Y P, Yu J H, Wang X, et al. Correlation analysis of fetal hemodynamic changes and pregnancy outcome in pregnant women with pregnancy induced hypertension by ultrasound[J]. Journal of Medical Imaging, 2018, 28(2): 308-312. |
| [9] |
元幼女. 高危妊娠晚期胎儿脐动脉及大脑中动脉血流动力学变化分析[J]. 中国乡村医药, 2018, 25(18): 51-52. Yuan Y N. Hemodynamic changes of umbilical artery and middle cerebral artery in high risk pregnancy[J]. China Rural Medicine, 2018, 25(18): 51-52. DOI:10.3969/j.issn.1006-5180.2018.18.030 |
| [10] |
谢许萍, 胡燕芳, 程志坚, 等. 超声监测脐带缠绕胎儿脐动脉及大脑中动脉血流在预测胎儿宫内窘迫中的应用[J]. 现代仪器与医疗, 2018, 24(6): 39-41. Xie X P, Hu Y F, Cheng Z J, et al. Application of ultrasonic monitoring of umbilical artery and middle cerebral artery blood flow in the prediction of fetal distress[J]. Modern Instruments and Medical Treatment, 2018, 24(6): 39-41. |
| [11] |
张佐炳, 张晓东, 林锦蓉. 彩色多普勒超声检测子宫动脉及脐动脉在预测晚发型胎儿宫内生长受限中的价值[J]. 临床超声医学杂志, 2018, 232(8): 56-59. Zhang Z B, Zhang X D, Lin J R. The value of color Doppler ultrasound in the detection of uterine artery and umbilical artery in the prediction of late-onset fetal intrauterine growth restriction[J]. Journal of Clinical Ultrasound Medicine, 2018, 232(8): 56-59. |
| [12] |
Feng Y, Liao S, Wei C, et al. Infiltration and persistence of lymphocytes during late-stage cerebral ischemia in middle cerebral artery occlusion and photothrombotic stroke models[J]. Journal of Neuroinflammation, 2017, 14(1): 248. DOI:10.1186/s12974-017-1017-0 |
| [13] |
洪丽莉, 吴庆梅, 高艳, 等. 孕晚期胎儿彩色多普勒超声血流多参数异常与妊娠不良结局的关系[J]. 临床超声医学杂志, 2017, 19(6): 432-432. Hong L L, Wu Q M, Gao Y, et al. The relationship between multiparameter abnormality of fetal color Doppler flow and adverse pregnancy outcome[J]. Journal of Clinical Ultrasound Medicine, 2017, 19(6): 432-432. DOI:10.3969/j.issn.1008-6978.2017.06.028 |
| [14] |
舒特标, 夏志新, 赖庆甜. 彩超检测高危妊娠晚期孕妇胎儿脐动脉及大脑中动脉血流动力水平的临床意义[J]. 当代医学, 2019, 25(28): 25-27. Shu T B, Xia Z X, Lai Q T. The clinical significance of color Doppler ultrasound in the detection of fetal umbilical artery and middle cerebral artery hemodynamics in high-risk pregnant women in the late pregnancy[J]. Contemporary medicine, 2019, 25(28): 25-27. DOI:10.3969/j.issn.1009-4393.2019.28.009 |
| [15] |
颜媛, 邹翰琴, 周克松, 等. 胎儿脐动脉、肾动脉及大脑中动脉血流动力学与胎儿宫内缺氧的相关性研究[J]. 四川医学, 2018, 39(9): 91-94. Yan Y, Zou H Q, Zhou K S, et al. Correlation between fetal umbilical artery, renal artery and middle cerebral artery hemodynamics and fetal intrauterine hypoxia[J]. Sichuan Medical Journal, 2018, 39(9): 91-94. |
| [16] |
赵金菊, 骆学东. 胎儿动脉MCA、MCA与UA的阻力指标在高血压产妇母婴结局预测价值[J]. 内蒙古医科大学学报, 2019, 41(4): 354-356, 359. Zhao J J, Luo X D. The predictive value of MCA, MCA and UA resistance indexes of fetal artery in maternal and infant outcome of hypertensive women[J]. Journal of Inner Mongolia Medical University, 2019, 41(4): 354-356, 359. |
| [17] |
杨超, 傅晓冬. 脐动脉、大脑中动脉血流联合胎心监护对预测重度子痫前期患者围生儿结局的价值[J]. 中国妇幼保健, 2019, 34(15): 3456-3459. Yang C, Fu X D. The value of umbilical artery, middle cerebral artery blood flow and fetal heart rate monitoring in predicting perinatal outcome of severe preeclampsia[J]. China Maternal and Child Health Care, 2019, 34(15): 3456-3459. |
| [18] |
李彬, 陈慧明, 张霞, 等. 胎儿脐动脉、肾动脉及大脑中动脉血流动力学预测晚孕期妊娠糖尿病妊娠结局的临床价值[J]. 中国医学创新, 2018, 15(17): 54-57. Li B, Chen H M, Zhang X, et al. The clinical value of fetal umbilical artery, renal artery and middle cerebral artery hemodynamics in predicting the pregnancy outcome of gestational diabetes mellitus in late pregnancy[J]. Chinese Medical Innovation, 2018, 15(17): 54-57. DOI:10.3969/j.issn.1674-4985.2018.17.014 |



